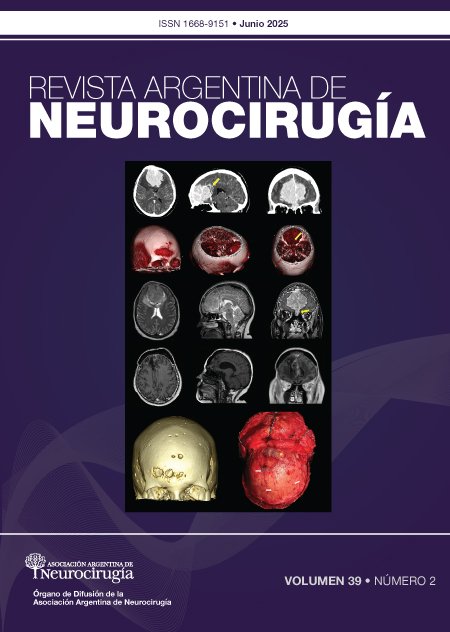
Malformaciones arteriovenosas múltiples
DOI:
https://doi.org/10.59156/revista.v39i02.740Palabras clave:
Hemorragia intracraneal, Malformación arteriovenosa cerebral múltiple, Síndrome de Rendu-Osler-Weber, Síndrome de Wyburn-MasonResumen
Introducción: las malformaciones arteriovenosas (MAVs) suelen ser lesiones únicas; en ocasiones pueden presentarse de forma múltiple, asociadas a enfermedades congénitas.
Objetivos: realizar una actualización bibliográfica sobre las MAVs cerebrales múltiples y analizar su prevalencia, asociación a síndromes congénitos y la casuística de nuestra institución.
Conclusión: las MAVs cerebrales múltiples son poco frecuentes y requieren de un equipo multidisciplinario en su abordaje debido a su alta asociación a síndromes congénitos. Esta entidad representó el 1.27% del total de MAVs tratadas en nuestra institución y el 1.75% según lo reportado en diferentes series de casos publicadas previamente en la literatura. Se encontró con mayor frecuencia asociada a síndromes congénitos; el síndrome de Rendu-Osler-Weber fue el más común, presente en el 50% de los casos.
Descargas
Referencias
Manzato LB, Vanzin JR, Frighetto L, Filho PM, Pedrolo E, Terciany MP, et al. Multiple cerebral arteriovenous malformation: report of two cases and treatment strategy. J Neurol Neurobiol, 2017; 3(1): 1-4.
Berman MF, Sciacca RR, Pile-Spellmann J, et al. The epidemiology of brain arteriovenous malformations. Neurosurgery, 2000; 47: 389-96.
ApSimon HT, Reef H, Phadke RV, Popovic EA. A population-based study of brain arteriovenous malformation: long-term treatment outcomes. Stroke, 2002; 33(12): 2794-2800.
Stapf C, Mast H, Sciacca RR, et al. The New York Island’s AVM study: design, study progress, and initial results. Stroke, 2003; 34(5): e29-33.
Al-Shahi R, Fang JS, Lewis SC, et al. Prevalence of adults with brain arteriovenous malformations: a community-based study in Scotland using capture-recapture analysis. J Neurol Neurosurg Psychiatry, 2002; 73(5): 547-51.
Morris Z, Whiteley WN, Longstreth WT Jr, et al. Incidental findings on brain magnetic resonance imaging: systematic review and meta-analysis. BMJ, 2009; 339: b3016.
Weber F, Knopf H. Incidental findings in magnetic resonance imaging of the brains of healthy young men. J Neurol Sci, 2006; 240: 81-4.
Ondra SL, Troupp H, George ED, Schwab K. The natural history of symptomatic arteriovenous malformations of the brain: a 24-year follow-up assessment. J Neurosurg, 1990; 73(3): 387-91.
Stapf C, Mast H, Sciacca RR, et al. Predictors of hemorrhage in patients with untreated brain arteriovenous malformation. Neurology, 2006; 66(9): 1350-5.
Crawford PM, West CR, Chadwick DW, et al. Arteriovenous malformations of the brain: natural history in unoperated patients. J Neurol Neurosurg Psychiatry, 1986; 49(1): 1-10.
Itoyama Y, Uemura S, Ushio Y, et al. Natural course of unoperated intracranial arteriovenous malformations: study of 50 cases. J Neurosurg, 1989; 71(6): 805-9.
Yamada S, Takagi Y, Nozaki K, et al. Risk factors for subsequent hemorrhage in patients with cerebral arteriovenous malformations. J Neurosurg, 2007; 107(5): 965-72.
Al-Shahi R, Warlow C. A systematic review of the frequency and prognosis of arteriovenous malformations of the brain in adults. Brain, 2001; 124: 1900-26.
Choi JH, Mast H, Sciacca RR, Hartmann A, Khaw AV, Mohr JP, Stapf C. Clinical outcome after first and recurrent hemorrhage in patients with untreated brain arteriovenous malformation. Stroke, 2006; 37(5): 1243-7.
van Beijnum J, van der Worp HB, Algra A, et al. Prevalence of brain arteriovenous malformations in first-degree relatives of patients with a brain arteriovenous malformation. Stroke, 2014; 45(11): 3231-5.
Gross BA, Du R. Natural history of cerebral arteriovenous malformations: a meta-analysis. J Neurosurg, 2013; 118(2): 437-43.
Brown RD, Wiebers DO, Forbes G, O’Fallon WM, Piepgras DG, Marsh WR, Maciunas RJ. The natural history of unruptured intracranial arteriovenous malformations. J Neurosurg, 1988; 68: 352-7.
da Costa L, Wallace MC, Ter Brugge KG, et al. The natural history and predictive features of hemorrhage from brain arteriovenous malformations. Stroke, 2009; 40: 100-5.
Graf CJ, Perret GE, Torner JC. Bleeding from cerebral arteriovenous malformations as part of their natural history. J Neurosurg, 1983; 58: 331-7.
Brown RD Jr, Wiebers DO, Torner JC, et al. Frequency of intracranial hemorrhage as a presenting symptom and subtype analysis: a population-based study of intracranial vascular malformations in Olmsted County, Minnesota. J Neurosurg, 1996; 85: 29-32.
Fults D, Kelly DL. Natural history of arteriovenous malformations of the brain: a clinical study. Neurosurgery, 1984; 15: 658-62.
Wilkins R. Natural history of intracranial vascular malformations of the brain: a review. Neurosurgery, 1985; 16: 421-30.
Robert T, Blanc R, Botta D, Ciccio G, Smajda S, Redjem H, Piotin M. Management of multiple cerebral arteriovenous malformations in a non-pediatric population. Acta Neurochir, 2016; 158(6): 1019-25.
Salcman M, Scholtz H, Numaguchi Y. Multiple intracerebral arteriovenous malformations: report of three cases and review of the literature. Surg Neurol, 1992; 38(2): 121-8.
Willinsky RA, Lasjaunias P, Terbrugge K, Burrows P. Multiple cerebral arteriovenous malformations (AVMs). Review of our experience from 203 patients with cerebral vascular lesions. Neuroradiology, 1990; 32: 207-11.
Bharatha A, Faughnan ME, Kim H, Pourmohamad T, Krings T, Bayrak-Toydemir P, Terbrugge KG. Brain arteriovenous malformation multiplicity predicts the diagnosis of hereditary hemorrhagic telangiectasia: quantitative assessment. Stroke, 2011; 43(1): 72-8.
Jessurun GAJ, Kamphuis DJ, van der Zande FHR, Nossent JC. Cerebral arteriovenous malformations in the Netherlands Antilles. Clin Neurol Neurosurg, 1993; 95(3): 193-8.
Boone CE, Caplan JM, Yang W, Ye X, Colby GP, Coon AL, Huang J. Hemorrhage risk and clinical features of multiple intracranial arteriovenous malformations. J Clin Neurosci, 2016; 23: 51-7.
Iizuka Y, Rodesch G, Garcia-Monaco R, Alvarez H, Burrows P, Hui F, Lasjaunias P. Multiple cerebral arteriovenous shunts in children: report of 13 cases. Childs Nerv Syst, 1992; 8(8): 437-44.
Fong D, Chan ST. Arteriovenous malformation in children. Childs Nerv Syst, 1988; 4: 199-203.
Moody RA, Poppen JL. Arteriovenous malformations. J Neurosurg, 1970; 32(5): 503-11.
Pohjola A, Oulasvirta E, Roine RP, Sintonen H, Hafez A, Koroknay-Pál P, Laakso A. Long-term health-related quality of life in 262 patients with brain arteriovenous malformation. Neurology, 2019; 10.1212/WNL.0000000000008196.
Perret G, Nishioka H. Arteriovenous malformations. J Neurosurg, 1966; 25(4): 467-90.
Yang W, Liu A, Hung AL, Braileanu M, Wang JY, Caplan JM, Huang J. Lower risk of intracranial arteriovenous malformation hemorrhage in patients with hereditary hemorrhagic telangiectasia. Neurosurgery, 2016; 78(5): 684-93.
Matsubara S, Mandzia JL, ter Brugge K, Willinsky RA, Faughnan ME. Angiographic and clinical characteristics of patients with cerebral arteriovenous malformations associated with hereditary hemorrhagic telangiectasia. AJNR Am J Neuroradiol, 2000; 21: 1016-20.
Yamashita K, Suzuki Y, Yoshizumi H, Takahashi J, Nogawa T. Multiple cerebral arteriovenous malformations: case report. Neurol Med Chir (Tokyo), 1993; 33(1): 24-7.
Putman CM, Chaulopka JC, et al. Exceptional multiplicity of cerebral arteriovenous malformations associated with hereditary hemorrhagic telangiectasia (Osler-Weber-Rendu syndrome). AJNR Am J Neuroradiol, 1996; 17: 1733-42.
Di Cosola M, Cazzolla AP, Scivetti M, Testa NF, Lo Muzio L, Favia G, Carrillo de Albornoz A, Bascones A. Síndrome de Rendu-Osler-Weber o telangiectasia hemorrágica hereditaria (HHT): descripción de dos casos y revisión de la literatura. Av Odontoestomatol, 2005; 21(6): 297-310.
Román G, Fisher M, Perl DP, Poser CM. Neurological manifestations of hereditary hemorrhagic telangiectasia (Rendu-Osler-Weber disease): report of 2 cases and review of the literature. Ann Neurol, 1978; 4(2): 130-44.
Brinjikji W, Iyer VN, Yamaki V, Lanzino G, Cloft HJ, Thielen KR, Wood CP. Neurovascular manifestations of hereditary hemorrhagic telangiectasia: a consecutive series of 376 patients during 15 years. AJNR Am J Neuroradiol, 2016; 37(8): 1479-86.
Haitjema T, Disch F, Overtoom TTC, Westermann CJJ, Lammers JWJ. Screening family members of patients with hereditary hemorrhagic telangiectasia. Am J Med, 1995; 99(5): 519-24.
Maher CO, Piepgras DG, Brown RD, Friedman JA, Pollock BE. Cerebrovascular manifestations in 321 cases of hereditary hemorrhagic telangiectasia. Stroke, 2001; 32(4): 877-82.
Krings T, Ozanne A, Chng SM, Alvarez H, Rodesch G, Lasjaunias PL. Neurovascular phenotypes in hereditary haemorrhagic telangiectasia patients according to age: review of 50 consecutive patients aged 1 day-60 years. Neuroradiology, 2005; 47: 711-20.
Shovlin CL, Guttmacher AE, Buscarini E, Faughnan ME, Hyland RH, Westermann CJJ, Plauchu H. Diagnostic criteria for hereditary hemorrhagic telangiectasia (Rendu-Osler-Weber syndrome). Am J Med Genet, 2000; 91(1): 66-7.
Dayani PN, Sadun AA. A case report of Wyburn-Mason syndrome and review of the literature. Neuroradiology, 2007; 49: 445-56.
Wyburn-Mason R. Arteriovenous aneurysm of mid-brain and retina, facial naevi and mental changes. Brain, 1943; 66: 163-90.
Turjman F, Massoud TF, Vinuela F, et al. Aneurysms related to cerebral arteriovenous malformations: superselective angiographic assessment in 58 patients. AJNR Am J Neuroradiol, 1994; 15: 1601-5.
Friedlander B. Arteriovenous malformations of the brain. N Engl J Med, 2007; 356: 2704-12.
Arce V JD, García B C, Otero J, Villanueva A E. Anomalías vasculares de partes blandas: imágenes diagnósticas. Rev Chil Radiol, 2007; 13(3): 109-21.
Hanieh A, Blumbergs P, Carney PG. Multiple cerebral arteriovenous malformations associated with soft-tissue vascular malformations. J Neurosurg, 1981; 54: 670-2.
Utsuki S, Kurata A, Miyasaka Y, Takano M, Ootaka H, Fujii K. Multiple arteriovenous malformations with hemorrhage. Acta Neurochir, 2002; 144(1): 97-101.
Kohmura E, Taki T, Tanioka T. Multiple intracerebral arteriovenous malformations in deep structure: case report. Neurol Med Chir (Tokyo), 1990; 30: 624-7.
Okada Y, Shima T, Nishida M, Yamane K. Bilateral symmetrical cerebral arteriovenous malformations in the basal ganglia: case report. Neurol Med Chir (Tokyo), 1992; 32: 88-92.
Tada T, Sugita K, Kobayashi S, Watanabe N. Supra- and infratentorial arteriovenous malformations with an aneurysmal dilatation: a case report. Neurosurgery, 1986; 19(5): 831-4.
Yoshimoto T, Kashiwaba T, Houkin K, Abe H. Spontaneous disappearance of arteriovenous malformation during staged treatment of multiple cerebral arteriovenous malformations: case report. Neurol Med Chir (Tokyo), 1996; 36: 812-4.
Liu R, Zhan Y, Piao J, Yang Z, et al. Treatments of unruptured brain arteriovenous malformations: a systematic review and meta-analysis. Medicine (Baltimore), 2021; 100(25): e26352.
Spetzler RF, Martin NA. A proposed grading system for arteriovenous malformations. J Neurosurg, 1986; 65(4): 476-83.
Lawton MT, Kim H, McCulloch CE, Mikhak B, Young WL. A supplementary grading scale for selecting patients with brain arteriovenous malformations for surgery. Neurosurgery, 2010; 66(4): 702-13.
Gallardo F, Marin C, Chang L, Diaz J, Bustamante J, Rubino P. Utilidad de las escalas de gradación en el tratamiento quirúrgico de las malformaciones. Rev Argent Neuroc, 2019; 33(1): 26-38.