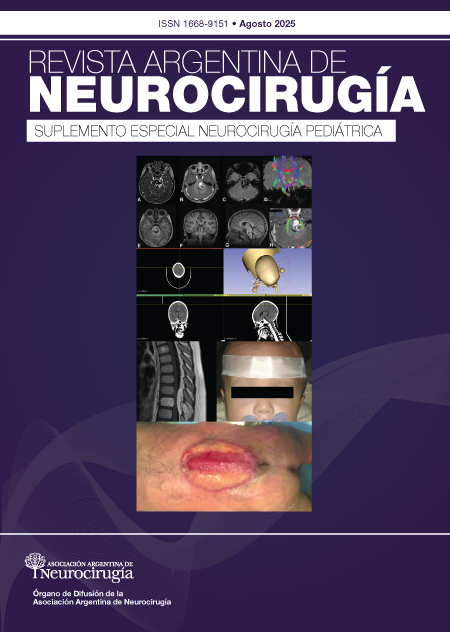
Cavernomas: análisis de 13 casos pediátricos
DOI:
https://doi.org/10.59156/revista.v0i0.682Palabras clave:
Cavernoma, Hemorragia intracraneal, Malformación cavernosa, Neurocirugía pediátricaResumen
Introducción: las malformaciones cavernosas (MC) o cavernomas (C) son malformaciones vasculares de bajo flujo, angiográficamente ocultas y con características por imágenes de resonancia magnética que pueden definir el tiempo de degradación de la hemoglobina e incluso pequeños niveles líquidos. Corresponden a una de las principales causas de sangrado cerebral en pediatría, y pueden ser esporádicas, o de tipo familiar y con lesiones múltiples. La remoción microquirúrgica se recomienda en casos sintomáticos y accesibles anatómicamente.
Objetivos: reportar nuestra serie de casos de cavernomas y comparar la información con la literatura publicada.
Material y métodos: estudio descriptivo retrospectivo de serie de casos de pacientes con diagnóstico de cavernomas entre abril de 2016 y abril de 2022, con revisión de historias clínicas, neuroimágenes, partes quirúrgicos y anatomopatológicos. Se recopilaron datos filiatorios, presentación clínica, localización, tipo de tratamiento, evolución y hallazgos por imágenes.
Resultados: se incluyeron 13 pacientes, 8 varones y 5 mujeres. Rango etario de 7 meses a 16 años (media 8.7 años); 3 pacientes (23%) con diagnóstico de cavernomatosis múltiple familiar; 6 supratentoriales corticales, 2 supratentoriales profundas, 3 en tronco encefálico, 1 cerebeloso y 1 medular. Doce casos (92%) debutaron con sangrado sintomático. Once (85%) requirieron cirugía, todos sintomáticos: 9 (82%) por primer sangrado y 2 (18%) en resangrado. El 100% resección total. Mejoría clínica postquirúrgica en el 91%. La media de seguimiento fue de 2.5 años. Se destacan 7 casos para su mayor análisis.
Conclusión: los cavernomas son entidades dinámicas que requieren seguimiento y debe considerarse la oportunidad quirúrgica, sobre todo en pacientes pediátricos con larga expectativa de vida. En lesiones sintomáticas y anatómicamente accesibles se logran resultados satisfactorios con resección quirúrgica completa.
Descargas
Referencias
Aslan A, Börcek AÖ, Demirci H, Erdem MB. Cerebral cavernous malformation presenting in childhood: a single-centered surgical experience of 29 cases. Clin Neurol Neurosurg, 2020; 194(1): 105830. DOI: https://doi.org/10.1016/j.clineuro.2020.105830
Porter PJ, Willinsky RA, Harper W, Wallace MC. Cerebral cavernous malformations: natural history and prognosis after clinical deterioration with or without hemorrhage. J Neurosurg, 1997; 87(2): 190-7. DOI: https://doi.org/10.3171/jns.1997.87.2.0190
Acciarri N, Galassi E, Giulioni M, Pozzati E, Grasso V, Palandri G, et al. Cavernous malformations of the central nervous system in the pediatric age group. Pediatr Neurosurg, 2009; 45(2): 81-104. DOI: https://doi.org/10.1159/000209283
International Society for the Study of Vascular Anomalies. ISSVA classification of vascular anomalies. Ear Nose Throat J, 2006; 85(6): 354. DOI: https://doi.org/10.1177/014556130608500602
Goldstein HE, Solomon RA. Epidemiology of cavernous malformations. In: Spetzler RF, Moon K, Almefty RO, editors. Handbook of Clinical Neurology. Amsterdam: Elsevier; 2017. p. 241-7. DOI: https://doi.org/10.1016/B978-0-444-63640-9.00023-0
Sawarkar DP, Janmatti S, Kumar R, Singh PK, Gurjar HK, Kale SS, et al. Cavernous malformations of central nervous system in pediatric patients: our single-centered experience in 50 patients and review of literature. Childs Nerv Syst, 2017; 33(9): 1525-38. DOI: https://doi.org/10.1007/s00381-017-3429-7
Bilginer B, Narin F, Hanalioglu S, Oguz KK, Soylemezoglu F, Akalan N. Cavernous malformations of the central nervous system (CNS) in children: clinico-radiological features and management outcomes of 36 cases. Childs Nerv Syst, 2014; 30(8): 1355-66. DOI: https://doi.org/10.1007/s00381-014-2442-3
Papadias A, Taha A, Sgouros S, Walsh AR, Hockley AD. Incidence of vascular malformations in spontaneous intra-cerebral haemorrhage in children. Childs Nerv Syst, 2007; 23(8): 881-6. DOI: https://doi.org/10.1007/s00381-007-0322-9
Bigi S, Capone Mori A, Steinlin M, Remonda L, Landolt H, Boltshauser E. Cavernous malformations of the central nervous system in children: presentation, treatment and outcome of 20 cases. Eur J Paediatr Neurol, 2011; 15(2): 109-16. DOI: https://doi.org/10.1016/j.ejpn.2010.09.004
Clatterbuck RE, Moriarity JL, Elmaci I, Lee RR, Breiter SN, Rigamonti D. Dynamic nature of cavernous malformations: a prospective magnetic resonance imaging study with volumetric analysis. J Neurosurg, 2000; 93(6): 981-6. DOI: https://doi.org/10.3171/jns.2000.93.6.0981
Hegde AN, Mohan S, Lim CCT. CNS cavernous haemangioma: “popcorn” in the brain and spinal cord. Clin Radiol, 2012; 67(4): 380-8. DOI: https://doi.org/10.1016/j.crad.2011.10.013
Bertalanffy H, Benes L, Miyazawa T, Alberti O, Siegel AM, Sure U. Cerebral cavernomas in the adult: review of the literature and analysis of 72 surgically treated patients. Neurosurg Rev, 2002; 25: 1-53. DOI: https://doi.org/10.1007/s101430100179
Karlsson B, Kihlström L, Lindquist C, Ericson K, Steiner L. Radiosurgery for cavernous malformations. J Neurosurg, 1998; 88(2): 293-7. DOI: https://doi.org/10.3171/jns.1998.88.2.0293
Kondziolka D, Lunsford LD, Kestle JRW. The natural history of cerebral cavernous malformations. J Neurosurg, 1995; 83(5): 820-4. DOI: https://doi.org/10.3171/jns.1995.83.5.0820
Salman RAS, Hall JM, Horne MA, Moultrie F, Josephson CB, Bhattacharya JJ, et al. Untreated clinical course of cerebral cavernous malformations: a prospective, population-based cohort study. Lancet Neurol, 2012; 11(3): 217-24. DOI: https://doi.org/10.1016/S1474-4422(12)70004-2
Zhang S, Ma L, Wu C, Wu J, Cao Y, Wang S, et al. A rupture risk analysis of cerebral cavernous malformation associated with developmental venous anomaly using susceptibility-weighted imaging. Neuroradiology, 2020; 62(1): 39-47. DOI: https://doi.org/10.1007/s00234-019-02274-1
Al-Holou WN, O’Lynnger TM, Pandey AS, Gemmete JJ, Thompson BG, Muraszko KM, et al. Natural history and imaging prevalence of cavernous malformations in children and young adults. J Neurosurg Pediatr, 2012; 9(2): 198-205. DOI: https://doi.org/10.3171/2011.11.PEDS11390
Suárez JC, Herrera EJ, Surus A, Pueyrredon FJ, Theaux R, Viano JC. Nuestro manejo de los cavernomas de tronco, de tálamo y ganglios basales. Rev Argent Neuroc, 2015; 29(4): 159-63.
Suárez JC, Viano JC, Herrera EJ, Calvo B, Altamirano C, Romero E, et al. Nuestra experiencia en el manejo de los cavernomas intracraneanos en la infancia. Rev Argent Neuroc, 2009; 23(2): 77-81.
Gross BA, Du R, Orbach DB, Scott RM, Smith ER. The natural history of cerebral cavernous malformations in children. J Neurosurg Pediatr, 2016; 17(2): 123-8. DOI: https://doi.org/10.3171/2015.2.PEDS14541
Li D, Hao SY, Tang J, Xiao XR, Jia GJ, Wu Z, et al. Clinical course of untreated pediatric brainstem cavernous malformations: hemorrhage risk and functional recovery. J Neurosurg Pediatr, 2014; 13(5): 471-83. DOI: https://doi.org/10.3171/2014.2.PEDS13487
Samanci Y, Ardor GD. Management of pediatric cerebral cavernous malformations with gamma knife radiosurgery: a report of 46 cases. Childs Nerv Syst, 2022; 38: 929-38. DOI: https://doi.org/10.1007/s00381-022-05485-9
Hirschmann D, Czech T, Roessler K, Krachsberger P, Paliwal S, Ciobanu-Caraus O, et al. How can we optimize the long-term outcome in children with intracranial cavernous malformations? A single-center experience of 61 cases. Neurosurg Rev, 2022; 45(5): 3299-313. DOI: https://doi.org/10.1007/s10143-022-01823-2
Mottolese C, Hermier M, Stan H, Jouvet A, Saint-Pierre G, Froment JC, et al. Central nervous system cavernomas in the pediatric age group. Neurosurg Rev, 2001; 24(2-3): 55-71. DOI: https://doi.org/10.1007/PL00014581
Di Rocco C, Lannelli A, Tamburrini G. Cavernous angiomas of the brain stem in children. Pediatr Neurosurg, 1997; 27(2): 92-9. DOI: https://doi.org/10.1159/000121233
Flemming KD, Link MJ, Christianson TJH, Brown RD. Prospective hemorrhage risk of intracerebral cavernous malformations. Neurology, 2012; 78(9): 632-6. DOI: https://doi.org/10.1212/WNL.0b013e318248de9b
Nikoubashman O, Di Rocco F, Davagnanam I, Mankad K, Zerah M, Wiesmann M. Prospective hemorrhage rates of cerebral cavernous malformations in children and adolescents based on MRI appearance. AJNR Am J Neuroradiol, 2015; 36(11): 2177-83. DOI: https://doi.org/10.3174/ajnr.A4427
Santos A, Rauschenbach L, Dinger TF, Saban DS, Chen B, Herten A, et al. Natural course of cerebral cavernous malformations in children: a five-year follow-up study. Brain Spine, 2021; 1: 100692. DOI: https://doi.org/10.1016/j.bas.2021.100692
Bottan JS, Rubino P. Manejo microquirúrgico de cavernomas supratentoriales. In: Rubino P, Arévalo R, Bottan JS, editors. Neurocirugía Vascular. Buenos Aires: Editorial Journal; 2021.
Nuñez M, Salas López E, Mural M, Neto MR, Rubino P. “Manejo microquirúrgico de cavernomas infratentoriales”. En: Rubino P, Arévalo R, Bottan JS, (eds.). Neurocirugía Vascular. Buenos Aires: Editorial Journal; 2021.
Srinivasan V, Gressot L, Daniels B, Jones J, Jea A, Lam S. Management of intracerebral hemorrhage in pediatric neurosurgery. Surg Neurol Int, 2016; 7(45): S1121-6. DOI: https://doi.org/10.4103/2152-7806.196919
Tyagi G, Sikaria A, Birua GJS, Beniwal M, Srinivas D. Surgical management of simultaneous supra- and infratentorial hemorrhages in a pediatric patient with multiple cavernomas. J Cerebrovasc Endovasc Neurosurg, 2022; 24(3): 262-6. DOI: https://doi.org/10.7461/jcen.2022.E2021.08.001
Akers A, Al-Shahi Salman R, Awad IA, Dahlem K, Flemming K, Hart B, et al. Synopsis of guidelines for the clinical management of cerebral cavernous malformations: consensus recommendations based on systematic literature review by the Angioma Alliance Scientific Advisory Board Clinical Experts Panel. Clin Neurosurg, 2017; 80(5): 665-80. DOI: https://doi.org/10.1093/neuros/nyx091
Bhardwaj RD, Auguste KI, Kulkarni AV, Dirks PB, Drake JM, Rutka JT. Management of pediatric brainstem cavernous malformations: experience over 20 years at the Hospital for Sick Children. J Neurosurg Pediatr, 2009; 4(5): 458-64. DOI: https://doi.org/10.3171/2009.6.PEDS0923
Jaikin MS, Musso A, Ayala N, Toledo AS. Abordaje interhemisférico contralateral: nota técnica. Rev Argent Neurocir, 2021; 35: 145-9. DOI: https://doi.org/10.59156/revista.v35i2.137
De Tribolet N, Kaech D, Perentes E. Cerebellar haematoma due to a cavernous angioma in a child. Acta Neurochir, 1982; [volumen]: 37-43. DOI: https://doi.org/10.1007/BF01401748
Fritschi JA, Reulen J, Spetzler RF, Zabramski JM. Cavernous malformations of the brain stem: a review of 139 cases. Acta Neurochir, 1994; 130: 35-4. DOI: https://doi.org/10.1007/BF01405501
Cavalheiro S, Yagmurlu K, da Costa MDS, Nicácio JM, Rodrigues TP, Chaddad-Neto F, et al. Surgical approaches for brainstem tumors in pediatric patients. Childs Nerv Syst, 2015; 31(10): 1815-40. DOI: https://doi.org/10.1007/s00381-015-2799-y
Cohen-Gadol AA, Jacob JT, Edwards DA, Krauss WE. Coexistence of intracranial and spinal cavernous malformations: a study of prevalence and natural history. J Neurosurg, 2006; 104(3): 376-81. DOI: https://doi.org/10.3171/jns.2006.104.3.376
Mespreuve M, Vanhoenacker F, Lemmerling M. Familial multiple cavernous malformation syndrome: MR features in this uncommon but silent threat. JBR-BTR, 2016; 100(1): 1-12. DOI: https://doi.org/10.5334/jbr-btr.938
Benedetti V, Canzoneri R, Perrelli A, Arduino C, Zonta A, Brusco A, et al. Next-generation sequencing advances the genetic diagnosis of cerebral cavernous malformation (CCM). Antioxidants, 2022; 11(7): 1-20. DOI: https://doi.org/10.3390/antiox11071294
Geraldo AF, Alves CAPF, Luis A, Tortora D, Guimarães J, Abreu D, et al. Natural history of familial cerebral cavernous malformation syndrome in children: a multicenter cohort study. Neuroradiology, 2023; 65(2): 401-414. DOI: https://doi.org/10.1007/s00234-022-03056-y
Pozzati E, Giuliani G, Nuzzo G, Poppi M, Piepgras DG, Hunt Batjer H. The growth of cerebral cavernous angiomas. Neurosurgery, 1989; 25: 92-7. DOI: https://doi.org/10.1227/00006123-198907000-00017