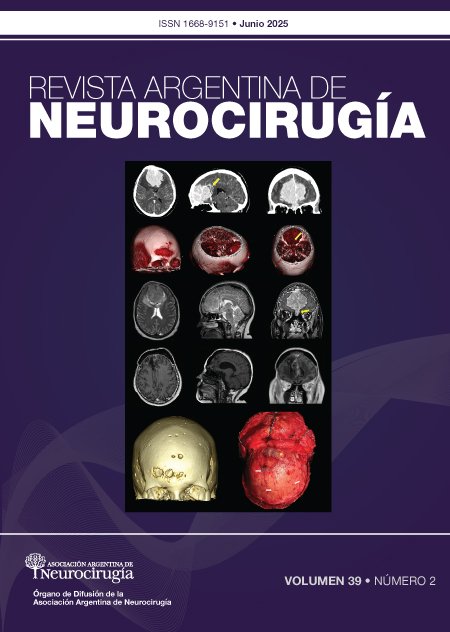
Multiple cerebral arteriovenous malformations
DOI:
https://doi.org/10.59156/revista.v39i02.740Keywords:
Intracranial hemorrhage, Multiple cerebral arteriovenous malformations, Rendu-Osler-Weber syndrome, Wyburn-Mason syndromeAbstract
Background: arteriovenous malformations (AVMs) are usually single lesions; occasionally, they can present in multiple forms associated with congenital diseases.
Objectives: to conduct a literature update on multiple cerebral AVMs and to analyze their prevalence, association with congenital syndromes, and the case series of our institution.
Methods: we conducted a cross-sectional, descriptive study based on the medical records of patients with cerebral AVMs between 2011 and 2021 at our institution. We identified those with multiple lesions (2 or more) and their association with congenital syndromes. A literature review was also conducted.
Results: according to an analysis of 13 publications including 5882 cases, multiple AVMs represent 1.75% of all patients with AVMs, and are associated with congenital disorders such as Rendu-Osler-Weber syndrome (ROWS) in 50% of cases and Wyburn-Mason syndrome (WMS) in 5.5–23% of patients. In our series, of 157 patients with cerebral AVMs, two presented with multiple lesions (1.27%), and one case was associated with ROWS.
Conclusion: multiple cerebral AVMs are rare and require a multidisciplinary team approach due to their high association with congenital syndromes. This entity represented 1.27% of all AVMs treated at our institution and 1.75%, according to analysis in various case series previously reported in the literature. It is most frequently associated with congenital syndromes, such as Rendu-Osler-Weber syndrome, in 50% of cases.
Downloads
References
Manzato LB, Vanzin JR, Frighetto L, Filho PM, Pedrolo E, Terciany MP, et al. Multiple cerebral arteriovenous malformation: report of two cases and treatment strategy. J Neurol Neurobiol, 2017; 3(1): 1-4.
Berman MF, Sciacca RR, Pile-Spellmann J, et al. The epidemiology of brain arteriovenous malformations. Neurosurgery, 2000; 47: 389-96.
ApSimon HT, Reef H, Phadke RV, Popovic EA. A population-based study of brain arteriovenous malformation: long-term treatment outcomes. Stroke, 2002; 33(12): 2794-2800.
Stapf C, Mast H, Sciacca RR, et al. The New York Island’s AVM study: design, study progress, and initial results. Stroke, 2003; 34(5): e29-33.
Al-Shahi R, Fang JS, Lewis SC, et al. Prevalence of adults with brain arteriovenous malformations: a community-based study in Scotland using capture-recapture analysis. J Neurol Neurosurg Psychiatry, 2002; 73(5): 547-51.
Morris Z, Whiteley WN, Longstreth WT Jr, et al. Incidental findings on brain magnetic resonance imaging: systematic review and meta-analysis. BMJ, 2009; 339: b3016.
Weber F, Knopf H. Incidental findings in magnetic resonance imaging of the brains of healthy young men. J Neurol Sci, 2006; 240: 81-4.
Ondra SL, Troupp H, George ED, Schwab K. The natural history of symptomatic arteriovenous malformations of the brain: a 24-year follow-up assessment. J Neurosurg, 1990; 73(3): 387-91.
Stapf C, Mast H, Sciacca RR, et al. Predictors of hemorrhage in patients with untreated brain arteriovenous malformation. Neurology, 2006; 66(9): 1350-5.
Crawford PM, West CR, Chadwick DW, et al. Arteriovenous malformations of the brain: natural history in unoperated patients. J Neurol Neurosurg Psychiatry, 1986; 49(1): 1-10.
Itoyama Y, Uemura S, Ushio Y, et al. Natural course of unoperated intracranial arteriovenous malformations: study of 50 cases. J Neurosurg, 1989; 71(6): 805-9.
Yamada S, Takagi Y, Nozaki K, et al. Risk factors for subsequent hemorrhage in patients with cerebral arteriovenous malformations. J Neurosurg, 2007; 107(5): 965-72.
Al-Shahi R, Warlow C. A systematic review of the frequency and prognosis of arteriovenous malformations of the brain in adults. Brain, 2001; 124: 1900-26.
Choi JH, Mast H, Sciacca RR, Hartmann A, Khaw AV, Mohr JP, Stapf C. Clinical outcome after first and recurrent hemorrhage in patients with untreated brain arteriovenous malformation. Stroke, 2006; 37(5): 1243-7.
van Beijnum J, van der Worp HB, Algra A, et al. Prevalence of brain arteriovenous malformations in first-degree relatives of patients with a brain arteriovenous malformation. Stroke, 2014; 45(11): 3231-5.
Gross BA, Du R. Natural history of cerebral arteriovenous malformations: a meta-analysis. J Neurosurg, 2013; 118(2): 437-43.
Brown RD, Wiebers DO, Forbes G, O’Fallon WM, Piepgras DG, Marsh WR, Maciunas RJ. The natural history of unruptured intracranial arteriovenous malformations. J Neurosurg, 1988; 68: 352-7.
da Costa L, Wallace MC, Ter Brugge KG, et al. The natural history and predictive features of hemorrhage from brain arteriovenous malformations. Stroke, 2009; 40: 100-5.
Graf CJ, Perret GE, Torner JC. Bleeding from cerebral arteriovenous malformations as part of their natural history. J Neurosurg, 1983; 58: 331-7.
Brown RD Jr, Wiebers DO, Torner JC, et al. Frequency of intracranial hemorrhage as a presenting symptom and subtype analysis: a population-based study of intracranial vascular malformations in Olmsted County, Minnesota. J Neurosurg, 1996; 85: 29-32.
Fults D, Kelly DL. Natural history of arteriovenous malformations of the brain: a clinical study. Neurosurgery, 1984; 15: 658-62.
Wilkins R. Natural history of intracranial vascular malformations of the brain: a review. Neurosurgery, 1985; 16: 421-30.
Robert T, Blanc R, Botta D, Ciccio G, Smajda S, Redjem H, Piotin M. Management of multiple cerebral arteriovenous malformations in a non-pediatric population. Acta Neurochir, 2016; 158(6): 1019-25.
Salcman M, Scholtz H, Numaguchi Y. Multiple intracerebral arteriovenous malformations: report of three cases and review of the literature. Surg Neurol, 1992; 38(2): 121-8.
Willinsky RA, Lasjaunias P, Terbrugge K, Burrows P. Multiple cerebral arteriovenous malformations (AVMs). Review of our experience from 203 patients with cerebral vascular lesions. Neuroradiology, 1990; 32: 207-11.
Bharatha A, Faughnan ME, Kim H, Pourmohamad T, Krings T, Bayrak-Toydemir P, Terbrugge KG. Brain arteriovenous malformation multiplicity predicts the diagnosis of hereditary hemorrhagic telangiectasia: quantitative assessment. Stroke, 2011; 43(1): 72-8.
Jessurun GAJ, Kamphuis DJ, van der Zande FHR, Nossent JC. Cerebral arteriovenous malformations in the Netherlands Antilles. Clin Neurol Neurosurg, 1993; 95(3): 193-8.
Boone CE, Caplan JM, Yang W, Ye X, Colby GP, Coon AL, Huang J. Hemorrhage risk and clinical features of multiple intracranial arteriovenous malformations. J Clin Neurosci, 2016; 23: 51-7.
Iizuka Y, Rodesch G, Garcia-Monaco R, Alvarez H, Burrows P, Hui F, Lasjaunias P. Multiple cerebral arteriovenous shunts in children: report of 13 cases. Childs Nerv Syst, 1992; 8(8): 437-44.
Fong D, Chan ST. Arteriovenous malformation in children. Childs Nerv Syst, 1988; 4: 199-203.
Moody RA, Poppen JL. Arteriovenous malformations. J Neurosurg, 1970; 32(5): 503-11.
Pohjola A, Oulasvirta E, Roine RP, Sintonen H, Hafez A, Koroknay-Pál P, Laakso A. Long-term health-related quality of life in 262 patients with brain arteriovenous malformation. Neurology, 2019; 10.1212/WNL.0000000000008196.
Perret G, Nishioka H. Arteriovenous malformations. J Neurosurg, 1966; 25(4): 467-90.
Yang W, Liu A, Hung AL, Braileanu M, Wang JY, Caplan JM, Huang J. Lower risk of intracranial arteriovenous malformation hemorrhage in patients with hereditary hemorrhagic telangiectasia. Neurosurgery, 2016; 78(5): 684-93.
Matsubara S, Mandzia JL, ter Brugge K, Willinsky RA, Faughnan ME. Angiographic and clinical characteristics of patients with cerebral arteriovenous malformations associated with hereditary hemorrhagic telangiectasia. AJNR Am J Neuroradiol, 2000; 21: 1016-20.
Yamashita K, Suzuki Y, Yoshizumi H, Takahashi J, Nogawa T. Multiple cerebral arteriovenous malformations: case report. Neurol Med Chir (Tokyo), 1993; 33(1): 24-7.
Putman CM, Chaulopka JC, et al. Exceptional multiplicity of cerebral arteriovenous malformations associated with hereditary hemorrhagic telangiectasia (Osler-Weber-Rendu syndrome). AJNR Am J Neuroradiol, 1996; 17: 1733-42.
Di Cosola M, Cazzolla AP, Scivetti M, Testa NF, Lo Muzio L, Favia G, Carrillo de Albornoz A, Bascones A. Síndrome de Rendu-Osler-Weber o telangiectasia hemorrágica hereditaria (HHT): descripción de dos casos y revisión de la literatura. Av Odontoestomatol, 2005; 21(6): 297-310.
Román G, Fisher M, Perl DP, Poser CM. Neurological manifestations of hereditary hemorrhagic telangiectasia (Rendu-Osler-Weber disease): report of 2 cases and review of the literature. Ann Neurol, 1978; 4(2): 130-44.
Brinjikji W, Iyer VN, Yamaki V, Lanzino G, Cloft HJ, Thielen KR, Wood CP. Neurovascular manifestations of hereditary hemorrhagic telangiectasia: a consecutive series of 376 patients during 15 years. AJNR Am J Neuroradiol, 2016; 37(8): 1479-86.
Haitjema T, Disch F, Overtoom TTC, Westermann CJJ, Lammers JWJ. Screening family members of patients with hereditary hemorrhagic telangiectasia. Am J Med, 1995; 99(5): 519-24.
Maher CO, Piepgras DG, Brown RD, Friedman JA, Pollock BE. Cerebrovascular manifestations in 321 cases of hereditary hemorrhagic telangiectasia. Stroke, 2001; 32(4): 877-82.
Krings T, Ozanne A, Chng SM, Alvarez H, Rodesch G, Lasjaunias PL. Neurovascular phenotypes in hereditary haemorrhagic telangiectasia patients according to age: review of 50 consecutive patients aged 1 day-60 years. Neuroradiology, 2005; 47: 711-20.
Shovlin CL, Guttmacher AE, Buscarini E, Faughnan ME, Hyland RH, Westermann CJJ, Plauchu H. Diagnostic criteria for hereditary hemorrhagic telangiectasia (Rendu-Osler-Weber syndrome). Am J Med Genet, 2000; 91(1): 66-7.
Dayani PN, Sadun AA. A case report of Wyburn-Mason syndrome and review of the literature. Neuroradiology, 2007; 49: 445-56.
Wyburn-Mason R. Arteriovenous aneurysm of mid-brain and retina, facial naevi and mental changes. Brain, 1943; 66: 163-90.
Turjman F, Massoud TF, Vinuela F, et al. Aneurysms related to cerebral arteriovenous malformations: superselective angiographic assessment in 58 patients. AJNR Am J Neuroradiol, 1994; 15: 1601-5.
Friedlander B. Arteriovenous malformations of the brain. N Engl J Med, 2007; 356: 2704-12.
Arce V JD, García B C, Otero J, Villanueva A E. Anomalías vasculares de partes blandas: imágenes diagnósticas. Rev Chil Radiol, 2007; 13(3): 109-21.
Hanieh A, Blumbergs P, Carney PG. Multiple cerebral arteriovenous malformations associated with soft-tissue vascular malformations. J Neurosurg, 1981; 54: 670-2.
Utsuki S, Kurata A, Miyasaka Y, Takano M, Ootaka H, Fujii K. Multiple arteriovenous malformations with hemorrhage. Acta Neurochir, 2002; 144(1): 97-101.
Kohmura E, Taki T, Tanioka T. Multiple intracerebral arteriovenous malformations in deep structure: case report. Neurol Med Chir (Tokyo), 1990; 30: 624-7.
Okada Y, Shima T, Nishida M, Yamane K. Bilateral symmetrical cerebral arteriovenous malformations in the basal ganglia: case report. Neurol Med Chir (Tokyo), 1992; 32: 88-92.
Tada T, Sugita K, Kobayashi S, Watanabe N. Supra- and infratentorial arteriovenous malformations with an aneurysmal dilatation: a case report. Neurosurgery, 1986; 19(5): 831-4.
Yoshimoto T, Kashiwaba T, Houkin K, Abe H. Spontaneous disappearance of arteriovenous malformation during staged treatment of multiple cerebral arteriovenous malformations: case report. Neurol Med Chir (Tokyo), 1996; 36: 812-4.
Liu R, Zhan Y, Piao J, Yang Z, et al. Treatments of unruptured brain arteriovenous malformations: a systematic review and meta-analysis. Medicine (Baltimore), 2021; 100(25): e26352.
Spetzler RF, Martin NA. A proposed grading system for arteriovenous malformations. J Neurosurg, 1986; 65(4): 476-83.
Lawton MT, Kim H, McCulloch CE, Mikhak B, Young WL. A supplementary grading scale for selecting patients with brain arteriovenous malformations for surgery. Neurosurgery, 2010; 66(4): 702-13.
Gallardo F, Marin C, Chang L, Diaz J, Bustamante J, Rubino P. Utilidad de las escalas de gradación en el tratamiento quirúrgico de las malformaciones. Rev Argent Neuroc, 2019; 33(1): 26-38.