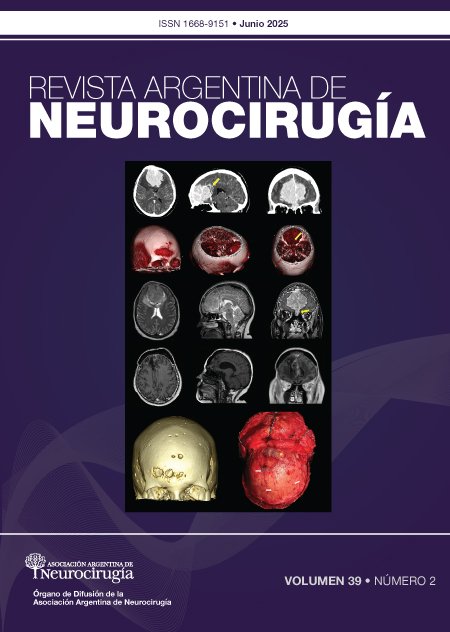
Aneurysmal subarachnoid hemorrhage and primary decompressive craniectomy: management guidelines based on 13 years of experience at a referral center
DOI:
https://doi.org/10.59156/revista.v39i02.718Keywords:
Clipping, Decompressive craniectomy, Morbidity and mortality, Subarachnoid hemorrhageAbstract
Background: decompressive craniectomy is an effective therapeutic tool for controlling intracranial hypertension, indicated both primarily based on clinical and imaging predictors, and later when hypertension becomes refractory. In the context of aneurysmal subarachnoid hemorrhage, hypertension may present immediately or delayed, associated with cerebral edema, hydrocephalus, hematomas, or infarcts due to vasospasm. In cases requiring urgent microsurgical clipping, the decision to combine decompressive craniectomy should be based on clinical status, preoperative imaging, and intraoperative findings, without delaying treatment of the ruptured aneurysm.
Objectives: to evaluate the indication for primary decompressive craniectomy in patients with subarachnoid hemorrhage undergoing microsurgical clipping and to identify predictors of early reintervention and their impact on functional outcome.
Methods: retrospective analysis of patients with SAH admitted to our center between 2011 and 2024 treated with clipping and requiring decompressive craniectomy either primary or within 48 hours of clipping. Management was analyzed in each case. The Chi-square test or Fisher's exact test was used, as appropriate, to establish the association between variables. Functional outcome was assessed at 6 months using the modified Rankin Scale (mRS).
Results: a total of 113 SAHs treated with clipping required decompressive craniectomy within the first 48 hours: 87.6% primary and 12.4% secondary. The indication was associated with poor neurological grade, presence of hydrocephalus, hematoma with mass effect, and brain herniation at the time of surgery. The presence of a hematoma with mass effect, poor neurological grade, and brain herniation at the end of clipping were statistically significantly associated with an unfavorable mRS. A "relaxed" brain at the end of clipping may underestimate cerebral edema and must be contextualized with other variables.
Conclusion: we present the institutional approach as a guideline for the management of these cases. This subgroup of patients is associated with high morbidity and mortality, so early identification of candidates for decompressive craniectomy could significantly modify their clinical course.
Downloads
References
Darkwah Oppong M, Golubovic J, Hauck EF, Wrede KH, Sure U, Jabbarli R. Decompressive craniectomy in aneurysmal subarachnoid hemorrhage: Who and when? – A systematic review and meta-analysis. Vol. 199, Clinical Neurology and Neurosurgery. Elsevier B.V.; 2020.
Brandecker S, Hadjiathanasiou A, Kern T, Schuss P, Vatter H, Güresir E. Primary decompressive craniectomy in poor-grade aneurysmal subarachnoid hemorrhage: long-term outcome in a single-center study and systematic review of literature. Neurosurg Rev. 2021 Aug 1;44(4):2153–62.
Hoh BL, Ko NU, Amin-Hanjani S, Hsiang-Yi Chou S, Cruz-Flores S, Dangayach NS, et al. 2023 Guideline for the Management of Patients With Aneurysmal Subarachnoid Hemorrhage: A Guideline From the American Heart Association/American Stroke Association. Stroke. 2023 Jul 1;54(7):E314–70.
Güresir E, Schuss P, Vatter H, Raabe A, Seifert V, Beck J. Decompressive craniectomy in subarachnoid hemorrhage. Neurosurg Focus. 2009 Jun;26(6):1–8.
Hunt WE, Hess RM. Surgical Risk as Related to Time of Intervention in the Repair of Intracranial Aneurysms.
Frontera JA, Claassen J, Schmidt JM, Wartenberg KE, Temes R, Connolly ES, et al. PREDICTION OF SYMPTOMATIC VASOSPASM AFTER SUBARACHNOID HEMORRHAGE: THE MODIFIED FISHER SCALE CLINICAL STUDIES [Internet]. Vol. 58. 2006. Available from: www.neurosurgery-online.com
Le Roux PD, Elliott JP, Newell DW, Grady MS, Richard Winn H. Predicting outcome in poor-grade patients with subarachnoid hemorrhage: a retrospective review of 159 aggressively managed cases. Vol. 85, J. Neurosurg. 1996.
Brandecker S, Hadjiathanasiou A, Kern T, Schuss P, Vatter H, Güresir E. Primary decompressive craniectomy in poor-grade aneurysmal subarachnoid hemorrhage: long-term outcome in a single-center study and systematic review of literature. Neurosurg Rev. 2021 Aug 1;44(4):2153–62.
Jabbarli R, Oppong MD, Dammann P, Wrede KH, El Hindy N, Özkan N, et al. Time Is Brain! Analysis of 245 Cases with Decompressive Craniectomy due to Subarachnoid Hemorrhage. World Neurosurg. 2017 Feb 1;98:689-694.e2.
Brouwers PJAM, Dippel ; D W J, Vermeulen ; M, Lindsay ; K W, Hasan ; D, Van Gijn J. Amount of Blood on Computed Tomography as an Independent Predictor After Aneurysm Rupture [Internet]. Available from: http://stroke.ahajournals.org/
Otani N, Takasato Y, Masaoka H, Hayakawa T, Yoshino Y, Yatsushige H, et al. Surgical outcome following decompressive craniectomy for poor-grade aneurysmal subarachnoid hemorrhage in patients with associated massive intracerebral or sylvian hematomas. Cerebrovascular Diseases. 2008 Dec;26(6):612–7.
Ota N, Noda K, Hatano Y, Hashimoto A, Miyazaki T, Kondo T, et al. Preoperative Predictors and Prognosticators After Microsurgical Clipping of Poor-Grade Subarachnoid Hemorrhage: A Retrospective Study. World Neurosurg. 2019 May 1;125:e582–92.
Bhattacharjee S, Rakesh D, Ramnadha R, Manas P. Subarachnoid Hemorrhage and Hydrocephalus. Vol. 69, Neurology India. Wolters Kluwer Medknow Publications; 2021. p. S415–9.
Van G1jn J, Hijdra A, Wijdicks FM, Van Crevel H. Acute hydrocephalus after aneurysmal subarachnoid hemorrhage. Vol. 63, J Neurosurg. 1985.