Recurrent mycotic cerebral aneurysm in a pediatric patient. Case report
DOI:
https://doi.org/10.59156/cwdcwe59Keywords:
Aneurysm, Endovascular, Mycotic, PseudoaneurysmAbstract
Background: cerebral aneurysms in pediatrics represent less than 1% of patients under 15 years of age. "Mycotic" aneurysms occur due to deterioration of the arterial wall, generating a blind "saculation" adjacent to its lumen due to the action of an infectious agent, predominantly bacteria, leading to infective endocarditis.
Objectives: to describe the distant presentation of a second mycotic aneurysm in a patient with leukemia and a history of invasive fungal infection due to Aspergillus.
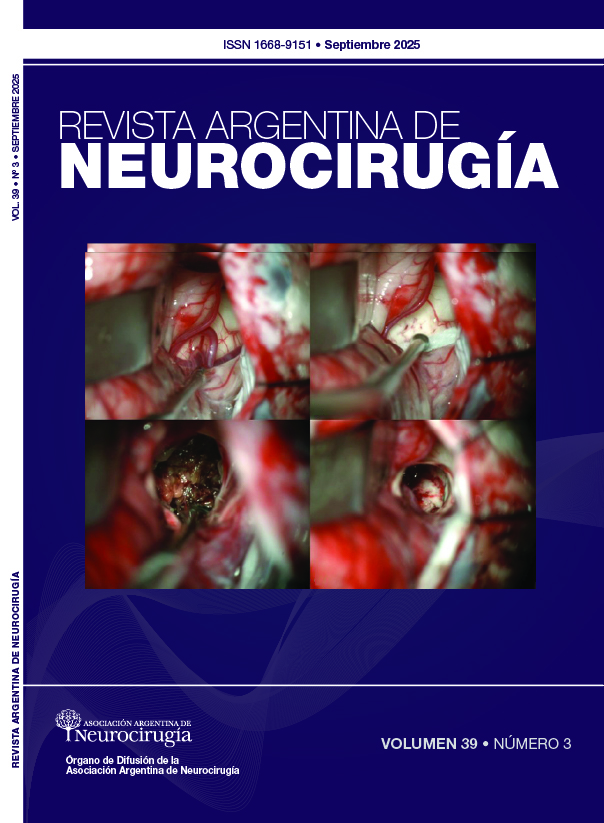
Case description: a16-year-old male patient with a history of acute lymphocytic leukemia presented with a right cerebellar abscess, with subsequent bleeding in the surgical bed secondary to a mycotic aneurysm of the posterior cerebral artery. With galactomannan rescue in the blood and a chest CT scan consistent with associated respiratory infection, treatment for invasive Aspergillus infection was initiated.
Surgery: endovascular treatment of the aneurysm was performed. Follow-up magnetic resonance imaging (MRI) revealed a fusiform dilation of the anterior communicating artery with involvement of the left A2 segment, associated with irregularity in the right M1 segment. A flow diverter was placed using endovascular therapy plus balloon plasty and coil placement.
Conclusion: endovascular treatment, complemented by antimicrobial therapy, requires prolonged follow-up with cerebral MRI to detect recurrence and reduce the risk of fatal bleeding.
Downloads
References
1. Heredia Gutierrez A, Carbarin M. Cerebral aneurysms in pediatrics: a case report and review of the literature. Scielo.2021;78(6):1-6. https://doi.org/10.24875/bmhim.20000406
2. Boissonneau S, Graillon T, Meyer M, Brunel H, Fuentes S, Dufour H. Intracranial Giant mycotic aneurysm without endocarditis and vasculitis: report of rare entity and review of literature. World Neurosurgery. 2018;119:353-7. https://doi.org/10.1016/j.wneu.2018.08.086
3. Ojeda A, Jimenez J, Gomez A, Montoya R, Sanguino R. Mycotic aneurism for septic embolism in a pediatric patient with acute linfoblastic leukemia. Rev Colomb Cancerol. 2019;23(4):158-62. https://doi.org/10.35509/01239015.119
4. Palacios A, Llorente A, Ordoñez O, Martinez A. Intracranial mycotic aneurysm in a 5 month-old infant with pneumococcal meningitis. Elsevier. 2017;35(3):267-9. doi: 10.1016/j.eimc.2016.03.008
5. Requejo F, Ceciliano A, Cardenas R, Villasante F, Jaimovich R, Zúccaro G. Aneurismas cerebrales en la infancia. Un solo nombre para diferentes enfermedades. Rev Argent Neurocir. 2010;24(3):131-3. https://aanc.org.ar/ranc/items/show/319
6. Escobar V, Montesinos A, Padilla F, Ramirez R, Mendizabal R. Aneurismas intracraneales en la infancia. Medigraphic. 2013;18(4):1-5 https://www.medigraphic.com/pdfs/arcneu/ane-2013/ane134h.pdf
7. Ducruet AF, Hickman ZL, Zacharia BE, Narula R, Grobelny BT, Gorski J, et al. “Intracranial infectious aneurysms: a comprehensive review”. Neurosurg Rev. 2010;33:37-46.
8. Mertens R, Kramer A, Valdés F, Garayar B, Irarrazaval M. Aneurismas micóticos y embolias múltiples en endocarditis infecciosa. Rev Med Chile. 1997. Disponible en: https://medicina.uc.cl/publicacion/aneurismas-micoticos-embolias-multiples-endocarditis-infecciosa/